
Rice University engineers have developed the first miniaturized brain stimulator shown to work in a human patient. Credit: Jeff Fitlow/Rice University
A small skull implant has positioned the Rice laboratory as a leader in neurotechnology research.
Rice University engineers have developed the smallest implantable brain stimulator demonstrated in a human patient. Thanks to pioneering magnetoelectric power transfer technology, the pea-sized device developed in the Rice lab of Jacob Robinson in collaboration with Motif Neurotech and clinicians Dr. Sameer Sheth and Dr. Sunil Sheth can be powered wirelessly via an external transmitter and used to stimulate the brain through the dura ⎯ the protective membrane attached to the bottom of the skull.
The device, known as the Digitally programmable Over-brain Therapeutic (DOT), could revolutionize treatment for drug-resistant depression and other psychiatric or neurological disorders by providing a therapeutic alternative that offers greater patient autonomy and accessibility than current neurostimulation-based therapies and is less invasive than other brain-computer interfaces (BCIs).
Technological Advancements and Research Findings
“In this paper, we show that our device, the size of a pea, can activate the motor cortex, which results in the patient moving their hand,” said Robinson, a professor of electrical and computer engineering and of bioengineering at Rice. “In the future, we can place the implant above other parts of the brain, like the prefrontal cortex, where we expect to improve executive functioning in people with depression or other disorders.”
Existing implantable technologies for brain stimulation are powered by relatively large batteries that need to be placed under the skin elsewhere in the body and connected to the stimulating device via long wires. Such design limitations require more surgery and subject the individual to a greater burden of hardware implantation, risks of wire breakage or failure, and the need for future battery replacement surgeries.
Rice University’s Jacob Robinson and his team of researchers have developed the smallest implantable brain stimulator demonstrated in a human patient that could revolutionize treatment for drug-resistant depression and other psychiatric or neurological disorders. Credit: Jeff Fitlow/Rice University
“We eliminated the need for a battery by wirelessly powering the device using an external transmitter,” explained Joshua Woods, an electrical engineering graduate student in the Robinson lab and lead author on the study published in 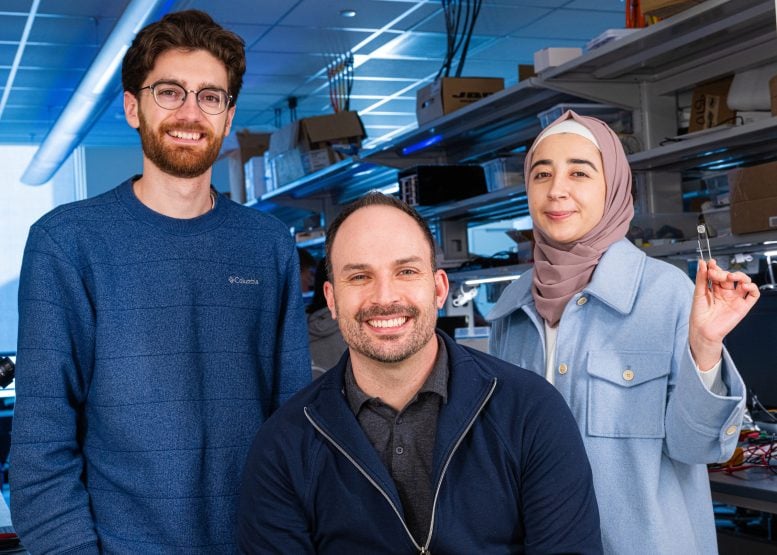
Joshua Woods (from left), Jacob Robinson and Fatima Alrashdan. Credit: Jeff Fitlow/Rice University
“When you think about a pacemaker, it’s a very routine part of cardiac care,” said Sheth, professor and vice-chair of research, McNair Scholar, and Cullen Foundation Endowed Chair of Neurosurgery at the Baylor College of Medicine. “In neurological and psychiatric disorders, the equivalent is deep brain stimulation (DBS), which sounds scary and invasive. DBS is actually quite a safe procedure, but it’s still brain surgery, and its perceived risk will place a very low ceiling on the number of people who are willing to accept it and may benefit from it. Here’s where technologies like this come in. A 30-minute minor procedure that is little more than skin surgery, done in an outpatient surgery center, is much more likely to be tolerated than DBS. So if we can show that it is about as effective as more invasive alternatives, this therapy will likely make a much larger impact on mental health.”
For some conditions, epilepsy for example, the device may need to be on permanently or most of the time, but for disorders such as depression and OCD, a regimen of just a few minutes of stimulation per day could suffice to bring about the desired changes in the functioning of the targeted neuronal network.
In terms of the next steps, Robinson said that on the research side, he is “really interested in the idea of creating networks of implants and creating implants that can stimulate and record, so that they can provide adaptive personalized therapies based on your own brain signatures.” From the therapeutic development standpoint, Motif Neurotech is in the process of seeking FDA approval for a long-term clinical trial in humans. Patients and caregivers can sign up on the Motif Neurotech website to learn when and where these trials will begin.
Reference: “Miniature battery-free epidural cortical stimulators” by Joshua E. Woods, Amanda L. Singer, Fatima Alrashdan, Wendy Tan, Chunfeng Tan, Sunil A. Sheth, Sameer A. Sheth and Jacob T. Robinson, 12 April 2024, Science Advances.DOI: 10.1126/sciadv.adn0858
The work was supported in part by The Robert and Janice McNair Foundation, the McNair Medical Institute, SciTechDaily