Researchers from KIST and Northwestern University developed a new device that monitors health conditions through sweat analysis without requiring physical activity. This device, which uses drug-stimulated sweat production, offers a painless alternative to blood tests and is particularly useful for individuals with limited mobility. (Artist’s concept.) Credit: SciTechDaily.com
Successful clinical testing on pediatric patients with cystic fibrosis using a flexible device enabling sweat gland stimulation and simultaneous biosensing. Two-year collaborative research between 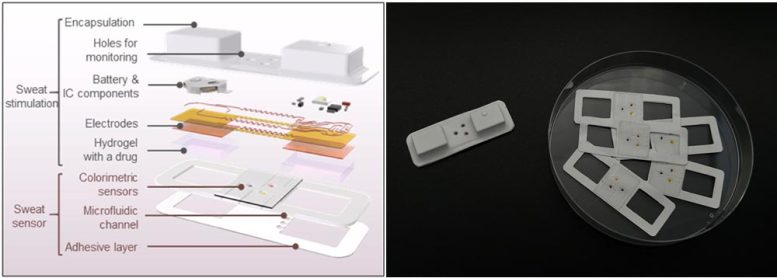
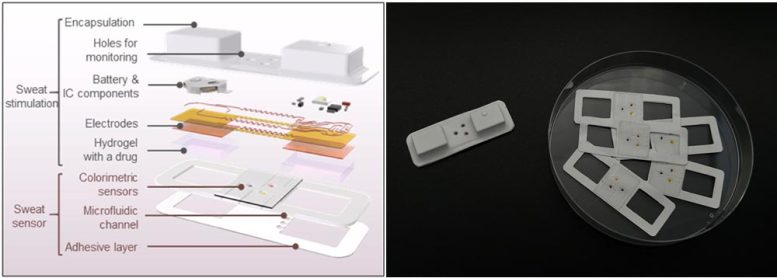
Illustration and photograph of the device capable of drug delivery for sweat induction and simultaneous monitoring of biomarkers in sweat. Credit: Korea Institute of Science and Technology
Development of a New Sweat Monitoring Device
Dr. Kim Joohee from the Bionics Research Center at the Korea Institute of Science and Technology (KIST) and Professor John A. Rogers from Northwestern University jointly announced the development of a convenient sweat monitoring device that does not require physical activity but delivers drug stimulation through the skin. Unlike previous methods that induced sweat through exercise, this device delivers drugs that stimulate sweat glands through the skin.
The research team developed a flexible device capable of delivering drugs to sweat glands by applying a current to a hydrogel containing drugs. This device, which is small and soft, can be easily attached to the skin. Sweat induced by the drug is collected in microfluidic channels within the device and analyzed for biomarkers using biosensors. This enables the analysis of biomarkers in sweat, reducing the need for cumbersome hospital visits for testing and lowering the risk of biomarker contamination during testing, thereby increasing 
A child with the traditional wired device attached to the left arm and the developed device adhered to the right arm, delivering drugs to stimulate sweat glands. Credit: Korea Institute of Science and Technology
Application in Pediatric Monitoring
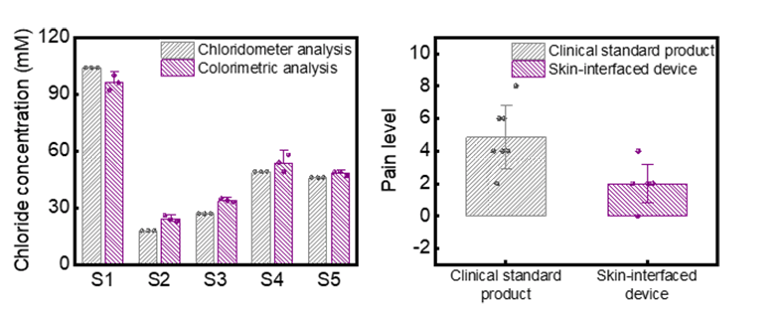
The device developed by the research team was attached to infants with cystic fibrosis, and the chloride concentration, a biomarker in sweat, was confirmed. The results were consistent with those obtained from traditional analysis methods using sweat collected in hospitals, with an accuracy of over 98%.
Additionally, the stability of the device on the skin was ensured by confirming skin temperature and pH values. Since cystic fibrosis mainly manifests during infancy, continuous monitoring of disease progression and physical condition is necessary. With this device, monitoring can be easily done at home, reducing the psychological and physical stress on pediatric patients and their caregivers.
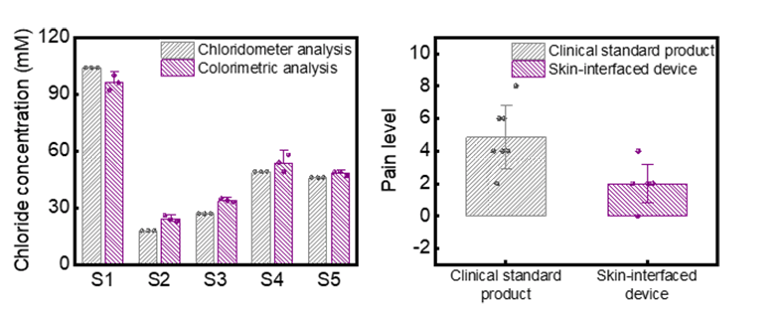
(Left) Graph showing over 98% agreement between the traditional diagnostic method and the developed device’s biomarker analysis results for five patients. (Right) Graph comparing the pain perception experienced by patients during disease monitoring using the traditional diagnostic method and the developed device. The graph indicates that the developed device causes less discomfort compared to the traditional diagnostic method. Credit: Korea Institute of Science and Technology
Potential Applications and Future Prospects
This newly developed device contributes to the expansion of non-invasive disease monitoring technology based on sweat in healthy adults as well. Furthermore, the technology of delivering drugs through the skin can be utilized not only to induce sweat but also to increase the delivery rate of drugs in localized areas such as skin conditions or wounds, thereby accelerating recovery.
Dr. Kim Joohee stated, “Through two years of collaborative research with Northwestern University, we have not only addressed the limitations of existing methods for inducing sweat but also achieved success in clinical research, bringing us one step closer to commercialization.” Professor John A. Rogers added, “We plan to conduct large-scale clinical studies and commercialization, including adults, in the future.”
Reference: “A skin-interfaced, miniaturized platform for triggered induction, capture and colorimetric multicomponent analysis of microliter volumes of sweat” by Joohee Kim, Seyong Oh, Da Som Yang, Larissa Rugg, Radhika Mathur, Sung Soo Kwak, Seonggwang Yoo, Shupeng Li, Evangelos E. Kanatzidis, Geumbee Lee, Hong-Joon Yoon, Yonggang Huang, Roozbeh Ghaffari, Susanna A. McColley and John A. Rogers, 23 February 2024, Biosensors and Bioelectronics.DOI: 10.1016/j.bios.2024.116166