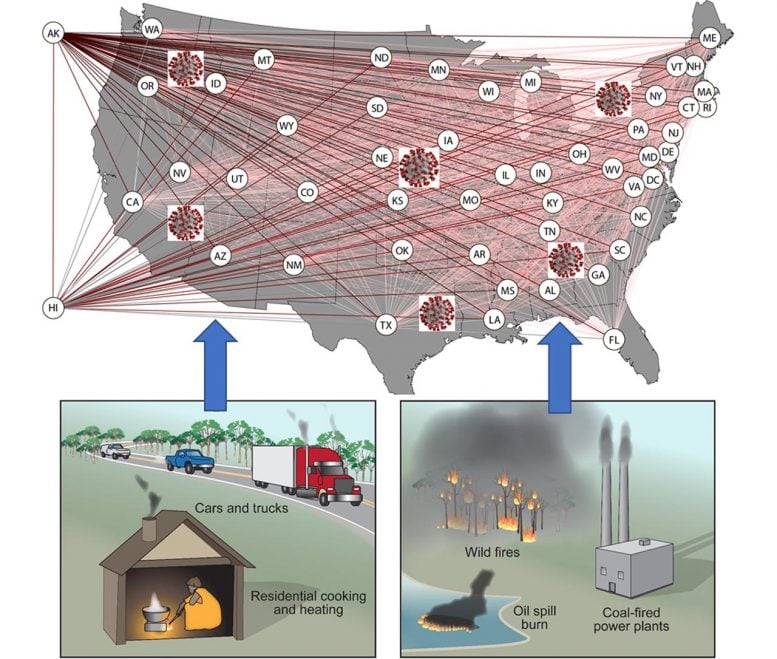
According to new research from the McKelvey School of Engineering at Washington University in St. Louis, pollution may bear part of the blame for the rapid proliferation in the United States of SARS-CoV-2, the virus responsible for the spread of COVID-19. Credit: Professor Rajan Chakrabarty, Washington University in St. Louis
Pollution and Pandemics: A Dangerous Mix
Research from Chakrabarty lab finds that as one goes, so goes the other — to a point.
The United States may have set itself up for the spread of a pandemic without even knowing it.
According to new research from the McKelvey School of Engineering at Washington University in St. Louis, pollution may bear part of the blame for the rapid proliferation in the United States of SARS-CoV-2, the virus responsible for the spread of COVID-19.
The research, from the lab of Rajan Chakrabarty, associate professor in the Department of Energy, Environmental & Chemical Engineering, was published online ahead of print in the journal Science of The Total Environment.
When it comes to how ill someone gets after contracting COVID-19, medical professionals believe that a person’s health — having certain medical conditions, for example — can play a vital role. When it comes to how fast the virus can spread through the community, it turns out the health of the environment is directly correlated to the basic reproduction ratio R0, which denotes the expected number of people each sick person can infect.
The reproduction ratio R0 of COVID-19 associates directly with the long-term ambient PM2.5 exposure levels. And the presence of secondary inorganic components in PM2.5 only makes things worse, according to Chakrabarty.
“We checked for more than 40 confounding factors,” Chakrabarty said. Of all of those factors, “There was a strong, linear association between long-term PM2.5 exposure and R0.”
PM2.5 refers to ambient particles with a diameter of 2.5 micrometers or less; at that size, they can enter a person’s lungs and cause damage. For this reason, PM2.5 can be detrimental to respiratory health. But how this relates to the spread of COVID-19 through a population had yet to be explored.
Chakrabarty and his graduate student Payton Beeler, both aerosol researchers who have done previous coronavirus modeling, became interested in the relationship after two papers were published in quick succession. First, a July paper in the journal Science found that levels of susceptibility to COVID-19 is a driving factor for the pandemic; it is more important than temperature, which researchers initially thought might play an outsized role.
Then in August, research published in the Journal of Infection found that the highest number of cases of COVID-19 with severe illness were in places with higher pollution levels.
“I was thinking, why, in the majority of the U.S. states, have we had such a rapid spread of the virus?” Chakrabarty said. Particularly in the earlier stages of the pandemic. “We wanted to confine our study to the point in time when the shutdown was in place. For the most part, people did remain confined from early March until the end of April.”
The team decided to look at places where R0 was greater than one — that’s the point at which one person can spread an illness to more than one person, and the illness takes off. In those places, they looked at 43 different factors — including population density, age distribution, even time delays in states’ stay-at-home orders.
Then, using pollution estimates across the U.S. between 2012 and 2017 published by Randall Martin, professor in the Department of Energy, Environmental & Chemical Engineering, the team looked for any relationships.
Modeling revealed an increase of almost 0.25 in R0 corresponding to a 10% increase in sulfate, nitrogen dioxide and ammonium, or SNA composition and an increase of 1 μg/m3 in PM2.5 mass concentrations, respectively.
They found these linear correlations to be strongest in places where pollution levels were well below National Ambient Air Quality Standards (NAAQS), the levels of air pollutants that are considered safe for humans.
“Annual mean PM2.5 national standards are set at or below 12 micrograms per cubic meter, below that you are supposed to be safe,” Chakrabarty said. “What we saw, the correlation we’re seeing is well below that standard.” In fact, they saw a rapid increase in R0 when PM2.5 exposure levels were below 6 micrograms per cubic meter.
Chakrabarty hypothesizes this initial increase in R0, which is followed by a plateau once levels hit 6 micrograms per cubic meter, is a result of initial changes in condition; when the air is free of PM2.5, an individual is unaffected. The initial exposure is the catalyst for change in lung health resulting in a change from non-susceptibility to susceptibility, which is reflected in the increasing R0.
And although there was no direct correlation between black carbon — a.k.a. soot — and R0, researchers did find a connection.
“Our collaborators at Saint Louis University suggested a mediation/moderation statistical approach,” a detailed analysis that looks at the way additional variables affect the outcome of the initial relationship. In this case, researchers looked at soot’s effect on R0, considering SNA’s effect.
“We found black carbon acts as a kind of catalyst. When there is soot present, PM2.5 has more of an acute effect on lung health, and therefore on R0.”
The mediation/moderation study was not superfluous — one of the common ways people are exposed to SNA is through pollution emitted from cars and coal-fired power plants. Both of which also emit soot.
“Although decades of strict air quality regulations in the U.S. have resulted in significant reductions of nitrogen dioxide levels,” the authors wrote in the paper’s conclusion, “recent reversal of environmental regulations which weaken limits on gaseous emissions from power plants and vehicles threaten the country’s future air quality scenario.”
“Instead of working to resolve this issue, these reversals may be setting us up for another pandemic,” Chakrabarty said.
Reference: “Ambient PM2.5 exposure and rapid spread of COVID-19 in the United States” by Rajan K. Chakrabarty, Payton Beeler, Pai Liu, Spondita Goswami, Richard D. Harvey, Shamsh Pervez, Aaronvan Donkelaar and Randall V. Martin, 9 November 2020, Science of The Total Environment.DOI: 10.1016/j.scitotenv.2020.143391
The authors have made their data and source codes available to the public.